Abstract
Background: Mutations in FMS like tyrosine kinase gene 3 (FLT3) are the most common genetic aberrations in acute myeloid leukemia (AML). Internal tandem duplications (ITD) are the most frequent FLT3 mutations, occurring in 20-30% of patients (pts) with newly diagnosed AML, and a minority are tyrosine kinase domain mutations. FLT3 mutation confers adverse prognosis in pts treated with standard chemotherapy (chemo) alone, and relapse risk is also higher compared to FLT3-wild type AML (HR-1.75). Studies of FLT3 inhibitors as monotherapy or in combination with chemo in the treatment of pts with FLT3-ITD relapsed/refractory (R/R) AML are associated with mixed results. No evidence synthesis has yet focused on the effect of FLT3 inhibitor alone in the treatment of R/R AML and high-risk myelodysplastic syndrome (HR-MDS). Hence, we analyzed the efficacy of various FLT3 inhibitors from different clinical trials used as monotherapy to treat pts with R/R AML and HR-MDS.
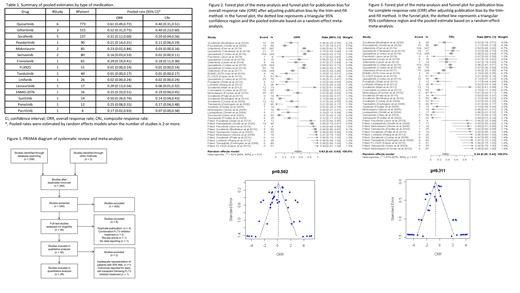
Methods: We conducted a systematic review and meta-analysis of clinical trials of FLT3 inhibitors for pts with R/R AML and HR-MDS. We searched EMBASE and PubMed for clinical trials published between 1/1/2000 and 5/26/2021 using a combination of keywords and subject headings related to FLT3 inhibitors and AML. Titles/abstracts and full texts were screened by two independent reviewers, with conflicts arbitrated by a third reviewer. Studies were included if they were (1) full-length published journal articles that (2) reported the results of single-arm or double-arm phase I/II/III clinical R/R AML or HR-MDS. Outcomes of interest were composite response rate (CRc=complete response + complete response with incomplete count recovery) and overall response rate (ORR).
Results: Thirty studies were included after the application of inclusion criteria (Figure 1). Two were excluded due to inadequate representation of pts with R/R AML and outcomes reported for stem cell transplant following FLT3 inhibitor use, respectively. Hence, 28 studies were included in the meta-analysis, with a total of 1927 pts. Quizartinib and sorafenib were the most frequently studied inhibitors (6 and 5 studies, respectively, Table 1). Heterogeneity testing was performed using Cochran's Q test and I 2 values. The Cochran's Q test p-value was less than 0.10 (p<0.01), and the I 2 value was more than 50% (I 2=87%), indicating the presence of heterogeneity. Thus, random-effects models were used. Asymmetry test was performed using Egger's linear regression test, which suggested the presence of publication bias (p=0.001; Figure 2). Thus, the trim-and-fill method was used to adjust for publication bias. Pooled ORR was 53% (95% CI, 43-63%) (Figure 2). Similarly, pooled CRc was 34% (95% CI, 26-44%, Figure 3). Pooled CRc and ORR were higher in studies involving quizartinib (40% and 61%, respectively) and gilteritinib (40% and 52%, respectively, Table 1). The CRc rates seen with FLT3 inhibitors are higher than the historical comparison of pts with FLT3-mutated-R/R AML treated with chemo only (CRc ~15%). This meta-analysis shows that FLT3 inhibitors as monotherapy leads to meaningful clinical responses in pts with FLT3-mutated-R/R AML.
Conclusion: Most FLT3 inhibitors are effective as monotherapy for the treatment of pts with FLT3-mutated-R/R AML. Pooled response rates are notably higher in studies involving second-generation FLT3 inhibitors, particularly quizartinib and gilteritinib. Though not conclusive, the efficacy spectrum of various FLT3 inhibitors in the R/R setting could help design future studies and guide appropriate treatment selection; however, further validation is needed. Prospective clinical trials are required to compare the effectiveness of newer generation FLT3 inhibitors in pts with FLT3-mutated-R/R AML.
Maciejewski: Bristol Myers Squibb/Celgene: Consultancy; Novartis: Consultancy; Regeneron: Consultancy; Alexion: Consultancy. Balasubramanian: Servier Pharmaceuticals: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal